A pregnancy complication is a health problem that arises during pregnancy. These can affect the mother’s health, the baby’s health, or both. Some women have complications during pregnancy, while others have health problems that could lead to concerns before becoming pregnant. To reduce the risk of pregnancy difficulties, women should seek medical attention before and during their pregnancy.1
According to the World Health Organization, every day, 800 women die as a result of childbirth problems. A pregnant woman from a developing nation is 36 times more likely than a pregnant woman from a developed country to experience pregnancy-related problems. Severe bleeding, hypertension, sepsis, unsafe abortion, and obstructed labour are the major causes of death in developing countries, all of which have simple, life-saving, and cost-effective treatments.2
What forms a part of the pregnancy complications list?
If you have a chronic illness or condition, talk to your doctor about how to avoid difficulties before becoming pregnant. If you are already pregnant, your doctor may need to monitor your pregnancy.
Apart from complications related to pregnancy such as subchorionic hemorrhage, placenta previa, amniotic fluid embolism and complications of childbirth such as breech presentation, prolonged labour etc., pre-existing diabetes, cancer, high blood pressure, infections, sexually transmitted infections (including HIV), kidney problems, epilepsy, and anemia are just a few examples of common diseases and conditions that might cause complications during your pregnancy.
Who is at risk for pregnancy complications?
The risk factors that could increase your problems include:
– having a child at an early age
– having a child at the age of 35 or older
– having an eating disorder such as anorexia
– poor immune system due to excess weight loss, stress or conditions such as HIV
– carrying multiples, such as twins or triplets
– history of preterm birth or pregnancy loss.
– cigarette smoking, illegal substance use (drugs), and alcohol consumption
What are the most common pregnancy problems?
It might be difficult to tell the difference between normal pregnancy symptoms and symptoms of complications. Although many problems are minor and do not progress, if you have any concerns during your pregnancy, you should always consult your doctor. With prompt treatment, the majority of pregnancy problems can be avoided.
The following are the most common pregnancy complications that women face:
1. Hypertension or high blood pressure:
When the arteries that transport blood from the heart to the organs and the placenta contract, high blood pressure develops. High blood pressure is linked to a higher risk of a variety of additional problems, including preeclampsia and seizures. It increases the chances of you delivering before your due date. This is referred to as premature labour. It also raises your chances of having a small baby. It’s critical to keep your blood pressure under control with medication and diet in order to have a healthy pregnancy.
2. Anemia:
Anemia is a condition characterised by low hemoglobin or iron content or low number of healthy red blood cells. This can be restored by treating the underlying cause of anemia. Anemia caused by pregnancy can make women feel fatigued and weak. Taking iron and folic acid supplements can help with this. Throughout your pregnancy, your doctor or nurse will monitor your iron levels.
3. Obesity and weight gain:
According to recent studies, the heavier a woman is in her pre-pregnancy, the higher her chance of pregnancy complications such as preeclampsia, gestational diabetes mellitus, stillbirth, and cesarean delivery. Obesity during pregnancy has also been linked to an increased need for health care and physician services, as well as longer hospital stays for delivery. Reducing excess weight before pregnancy increases the likelihood of a healthier pregnancy.
4. Gestational diabetes:
When your body can’t process sugars properly during pregnancy, you have gestational diabetes. This results in blood sugar levels that are higher than normal leading to health complications for both mother and baby. To help control blood sugar levels, some women will need to change their meal plans. Others may require the use of insulin to maintain blood sugar control. Frequently, gestational diabetes disappears after the birth of the baby.
5. Infections:
Many infections, such as the common cold or a passing stomach bug, are protected from your baby during pregnancy. However, you, your baby, or both of you can suffer serious health consequences from some infections. You can avoid infections by taking simple precautions like washing your hands and avoiding uncooked or street foods. You won’t always be able to tell whether you have an infection because you won’t feel sick. Consult your doctor if you suspect you have an infection or are at risk.
Infections with HIV, viral hepatitis, STIs, and tuberculosis can all affect pregnancy and have serious consequences for the mother, her pregnancy outcomes, and her baby. Many negative consequences can be avoided by screening and treating these infections, as well as immunizations against viruses like hepatitis B and the human papillomavirus (HPV).
6. Preterm labour:
When you go into labour before week 37 of your pregnancy, it is known as preterm labour. This may happen before your baby’s organs, such as the lungs and brain, have completed their development. Certain medications have the ability to stop labour. Consult your doctor to know the treatment options available for you.
7. Preeclampsia:
Toxemia is another name for preeclampsia. It happens after the first 20 weeks of pregnancy and results in excessive blood pressure as well as probable kidney problems. The birth of the baby and placenta is the recommended treatment for preeclampsia to prevent the disease from progressing. Your doctor will talk to you about the risks and benefits of having a baby at a specific time. If you’re 37 to 40 weeks pregnant, your doctor may decide to induce labour.
If it’s too soon to deliver your baby, your doctor will need to maintain a consistent eye on both you and your child. If you are not full-term, they may prescribe medications to help lower your blood pressure and help the baby mature. You may be admitted to the hospital for observation and treatment.
How to prevent pregnancy complications?
It is not possible to prevent all pregnancy-related complications. The following steps could help you have a healthy pregnancy and prevent a high-risk pregnancy.
- If you are planning to get pregnant, consult your doctor in advance to help you prepare. For instance, if you already have a medical problem, your doctor may recommend adjusting your treatment plan to prepare for pregnancy.
- Consume a balanced diet with plenty of fruits, vegetables, lean protein, and fibre.
- Take prenatal vitamins every day.
- Attending all the scheduled prenatal appointments, including those with a specialist, is advisable.
- You will have to quit smoking, in case you smoke.
- Avoid using illegal drugs and consumption of alcohol.
- Consult your doctor to decide if you should continue taking the medications you’re already taking or if you should stop taking them.
- Lower your stress levels. Listening to music and yoga are two ways to reduce stress.3 4
What are the early pregnancy complications?
Here are some symptoms you should pay closer attention to during the early months of pregnancy:
• Vaginal bleeding
While some spotting is normal, moderate to heavy bleeding may indicate a miscarriage or ectopic pregnancy. Bleeding and back or abdominal pains that resemble period cramps can indicate a threatened miscarriage. If it is along with sharp, lower abdomen pain, it could be a sign of ectopic pregnancy.
Your doctor will probably conduct some blood tests, an ultrasound, and an examination based on your symptoms. Even though some spotting or light bleeding is not a severe problem, you should not ignore it if it is associated with cramping, heavy bleeding or abdominal pain.
• Excessive nausea and vomiting
During your first trimester, it’s common to have some nausea and vomiting. However, you should pay attention if it’s severe or makes you more dehydrated. Vomiting that interferes with your daily activities might cause electrolyte imbalance, dehydration, weight loss, and dizziness. You may need hospitalisation to treat the dehydration.
There are many medications you can take to manage nausea. While nausea and vomiting are common during pregnancy, the extremes can cause problems. Most women who experience nausea and vomiting during the first trimester of their pregnancies go on to have a normal, healthy pregnancy.
• High fever
A fever that exceeds 38.3 degrees celsius during pregnancy could indicate an infection that could harm the baby. Fevers during pregnancy, along with rash and joint pain, could be a sign of an infection (like parvovirus, toxoplasma, and cytomegalovirus (CMV)). CMV is the most common cause of congenital deafness, which is not as rare as we believe. Speak to your doctor if you get rashes, joint pain, a fever, upper respiratory symptoms, a body ache, or flu-like symptoms.
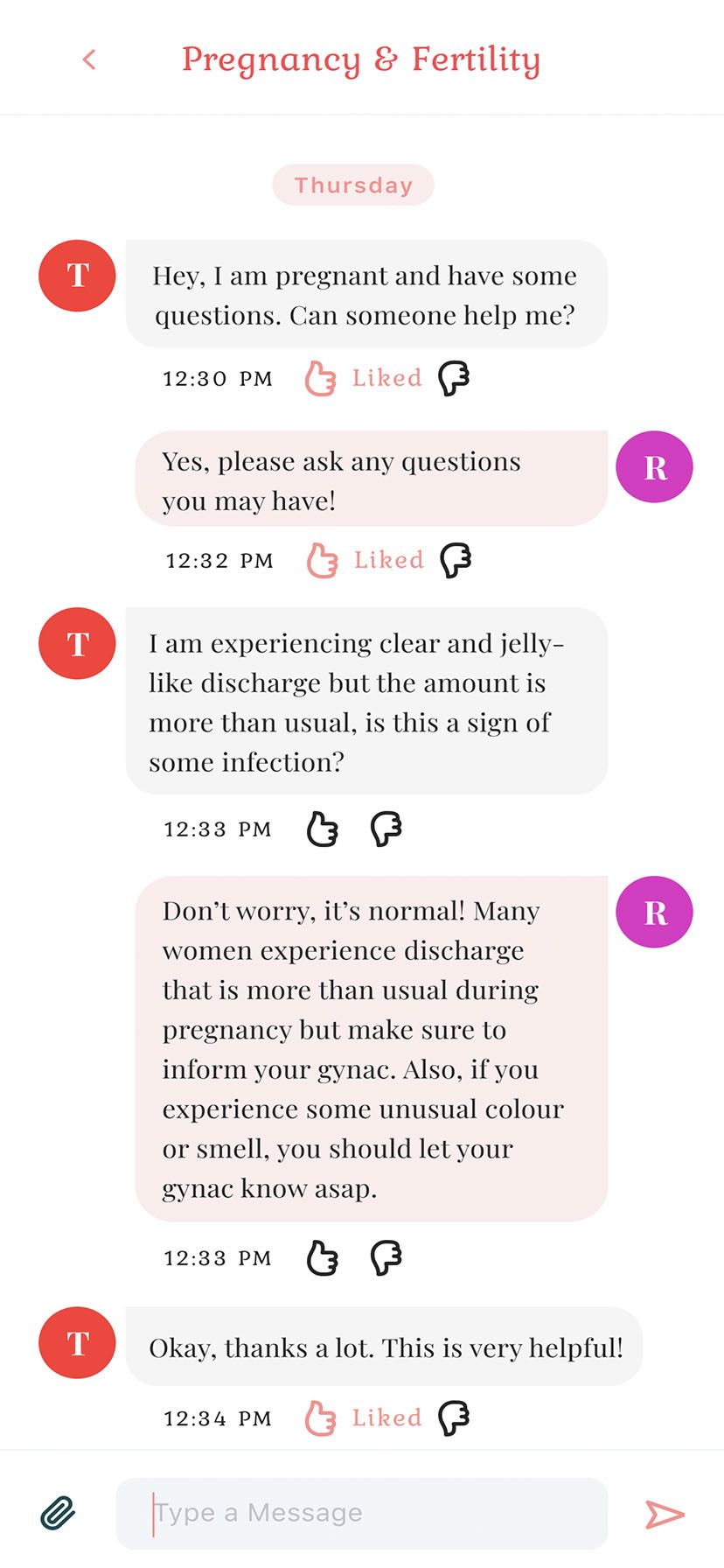
• Vaginal discharge and itching
It’s normal to have some vaginal discharge. However, in some cases, it may be due to fungal infections which are easily treated. In other cases, these may be symptoms of STIs that can have severe consequences on a pregnancy. If it is an infection, it could be harmful to the baby. Inform your doctor because if there is a problem, treating it can help your unborn baby.
• Flare-ups of chronic diseases
Pregnant women having pre-existing conditions, such as thyroid disease, diabetes, high blood pressure, asthma and lupus, should keep track of any changes in their health during pregnancy. If the underlying condition is flaring up and not controlled, it can seriously affect the health of you and your baby. There is an increased risk of miscarriage if your thyroid hormone level is too high or too low. Similarly, fetal abnormalities can increase your risk of miscarriage if your blood sugar levels are not monitored.5
What are the minor complications of pregnancy?
The minor complications of pregnancy are:
• Heartburn
Heartburn and reflux esophagitis are common, particularly in the last month or two months before delivery. Reflux esophagitis is a condition, where the pregnancy hormone relaxes the muscle that prevents food from the stomach from going back to the food pipe. It causes leakage of the acids in the stomach into the lower part of the food pipe, which causes heartburn. Eating small and frequent meals, sleeping on the left side can help ease the problem.
• Sleep deprivation or insomnia
Sleep deprivation is also frequent in the near term. It is possible to improve this situation by eating a light meal before going to bed and getting enough exercise during the day.
• Back pain
It is almost universal in women during their pregnancy. You can reduce it by maintaining a proper posture, footwear, and regular exercise during and after pregnancy. Always consult your doctor before starting a new workout routine. Relaxation exercises can ease back pain.
• Vaginal infection
Vaginal infection and itching are common in many women. The hormonal changes that occur during pregnancy make a woman more prone to infection, especially if she has diabetes. It is necessary to control blood sugar levels to prevent repeated infections. Vaginal pills can be used to treat this condition. Hence, you should consult your doctor without any hesitation.6
What are the most common complications of twin pregnancy?
Multiple pregnancies can have an increased risk of complications. The most common complications of a twin pregnancy are as follows:
• Preterm labour and birth
Over 60% of twins and nearly all higher-order multiples are premature (born before 37 weeks). The greater the number of fetuses in the pregnancy, the higher the chance of premature birth. These babies frequently weigh less than 2,500 grams at birth and may require help breathing, eating, fighting infection, and maintaining body temperature. Babies born before 28 weeks of pregnancy are especially vulnerable. Many of their organs might not be fully developed and unprepared for life outside the mother’s uterus. A neonatal intensive care unit (NICU) is needed to care for many multiple-birth babies.
• Gestational hypertension
Pregnant women with more than one fetus are more than twice as likely to experience high blood pressure. This condition frequently develops earlier and is more severe than pregnancy with one baby. Additionally, it is more likely to cause placental abruption (early detachment of the placenta).
• Anemia
Anemia is more than twice as common in multiple pregnancies compared to a pregnancy with a single baby.
• Birth abnormalities
Multiple birth babies are roughly twice as likely to have congenital (present at birth) abnormalities, such as cardiac, gastrointestinal, and neural tube abnormalities.
• Miscarriage
In multiple pregnancies, the vanishing twin syndrome is more likely to occur, wherein more than one fetus is detected but vanishes (or is miscarried), usually in the first trimester. It may or may not cause any bleeding. Even in the later trimesters, there is a higher risk of miscarriage.
• Twin-to-twin transfusion syndrome
The placenta disorder known as twin-to-twin transfusion syndrome (TTTS) develops in identical twins who share a placenta. Blood vessels connect within the placenta, and direct blood flows from one fetus to the other. Hence, blood is transferred from one fetus to the other via blood vessel connections in a shared placenta. The recipient fetus gradually receives too much blood, overloading the cardiovascular system and causing excessive amniotic fluid to develop. The smaller donor fetus receives insufficient blood and has little amniotic fluid. It occurs in approximately 15% of twins with a shared placenta.
• Abnormal amounts of amniotic fluid
Multiple pregnancies are more likely to experience amniotic fluid abnormalities, particularly when twins share a placenta.
• Cesarean delivery
Abnormal positions of the fetus can increase the chances of cesarean birth.
• Postpartum hemorrhage
In many multiple pregnancies, the mother is at risk for bleeding after delivery due to the large placental area and over-distended uterus.7
What are the rare pregnancy complications?
Here are some of the rare pregnancy complications:
• Selective Intrauterine Growth Restriction (sIUGR)
Identical twin pregnancies can result in a condition known as selective intrauterine growth restriction (sIUGR). It occurs when the placenta is not distributed evenly between the twins. Therefore, due to this imbalance, one twin may become malnourished. It causes complications in 10% to 15% of identical twin pregnancies. Your doctor will monitor the fetus and treat this condition.
• Congenital Diaphragmatic Hernia (CDH)
CDH is a condition that happens when there is a hole in the diaphragm (a thin muscle sheet separating the chest from the abdomen). When this gap arises during the development of a fetus in the womb, the colon, stomach, or even the liver can travel into the chest cavity, which can cause respiratory issues. It is caused when the process that leads to the formation of the diaphragm is disrupted, which can sometimes cause chromosomal and genetic disorders. A baby with CDH may undergo surgery after the delivery to reverse the lung damage caused due to compression of the lungs.
• Lower Urinary Tract Obstruction (LUTO)
LUTO is a rare fetal condition which happens when there is a blockage in the urinary tract of the developing fetus. LUTO occurs when the flow of urine exiting the body is blocked at the lower urinary tract, which causes swelling in the parts of the urinary tract. It can lead to permanent kidney damage over time. It is caused due to problems in the fetal chromosomes, genetic disorders, or parts of the urethra being too narrow or completely blocked. It can be treated through surgery, and various treatment options are available depending on the location of the urinary blockage.
• Twin-to-Twin Transfusion Syndrome (TTTS)
TTTS is a rare pregnancy condition that affects identical twins or other multiples. It develops in identical twin pregnancies where the twins share the same placenta and a network of blood vessels that supply oxygen and nutrients for the development of the womb.
The vessel connections within the placenta are not always equally dispensed, leading to an imbalance in blood exchange between the twins. The donor twin gives more blood than it receives, leading to malnutrition. The recipient twin receives too much blood and is prone to heart overwork and other cardiac problems.
• Twin Reversed Arterial Perfusion (TRAP)
TRAP is a rare condition in identical twin pregnancies. It develops when the cardiac system of one twin does the work of supplying blood for both. However, the twin that gives the blood is at risk for cardiac failure due to increased pumping. The other twin is born without a heart or is underdeveloped. It generally has a poorly developed body and may be missing a head, limbs, or torso.
• Ectopic pregnancy
Ectopic or tubal pregnancy is a pregnancy that occurs outside the uterus, generally in a fallopian tube. In rare cases, an ectopic pregnancy can develop in the ovary, cervix, or abdomen. It can be due to an infection or scar tissue or unexplained causes. It can be treated in many ways. Treatment is determined by whether the fallopian tube has ruptured, the stage of the pregnancy, and your hormone levels.
• Twin Anemia Polycythemia Sequence (TAPS)
TAPS is a type of twin-to-twin transfusion syndrome (TTTS) that can cause complications in identical twin pregnancies. It is a rare condition that arises when there is an unequal blood count between the twins inside the womb. Due to unequal blood counts, the twins have an imbalance in red blood cells and hemoglobin. It means that one twin is not getting enough oxygen and nutrients to develop properly. TAPS can develop randomly or due to incomplete laser surgery to treat TTTS.
• Fetal hydrothorax
It refers to the abnormal buildup of fluid inside the chest of a fetus, which may be present in various parts of the lungs. This fluid can compress the lungs, which may not allow oxygen intake at a normal level. It can even move the heart, which causes trouble for the fetus to receive and pump blood, causing heart failure.8
Call your doctor when:
If you’re pregnant, don’t hesitate to contact your doctor if you notice any unusual symptoms. If you have any of the following symptoms, call your doctor immediately to avoid any high-risk pregnancy complications – vaginal bleeding, sudden swelling of the hands or face, abdominal pain, fever, severe headaches, dizziness, persistent vomiting, or blurred vision.
If you notice your baby moving less frequently than usual during the third trimester, you should contact your doctor.9